Care1st Member Migration to Arizona Complete Health-Complete Care Plan
Date: 08/19/21
Background: In 2020, Arizona Complete Health’s parent company, Centene Corporation, completed the purchase of Wellcare, which includes Care1st Health Plan Arizona. As part of this change, Care1st Medicaid members in Maricopa, Gila and Pinal counties will become Arizona Complete Health-Complete Care Plan (AzCH-Complete Care Plan) members as of October 1, 2021. AHCCCS recently sent the impacted Care1st members a notice regarding this change and allowing members to select another AHCCCS plan if they chose. 
Questions and Answers
- Question: Do I need to do anything about this change?
- Answer: No, there is nothing you need to do. This agreement has been approved by AHCCCS for a 10/1/21 effective date.
- Question: What impact will this change have on my practice?
- Answer: There will be very little impact to you. Nearly all of the providers in the Care1st network are also contracted with AzCH-Complete Care Plan. If you are not part of the AzCH-Complete Care Plan network or are unsure about your status, please reach out to the AzCH-Complete Care Plan Contracting Team via email: azchcontracts@azcompletehealth.com.
- Question: Where is this change taking place?
- Answer: This change is taking place only in the Central Geographic Service Area, which is Maricopa, Pinal and Gila Counties. Care1st will continue to operate in the Northern GSA after 10/1/2021: Mohave, Coconino, Navajo, Apache and Yavapai Counties.
- Question: Will Care1st members remain with their service providers?
- Answer: Care1st and AzCH-Complete Care Plan have been working to minimize any impact to Care1st members. Most Care1st members will have access to their same providers. However, some members may need to be assigned to a different PCP or end up transitioning to a different specialist provider. If a member is assigned to a different PCP or Dental Home, they will be notified in writing in October. Some differences between the Care1st and AzCH-Complete Care Plan networks include:
- The Dental Administrator will change from DentaQuest to Envolve Benefit Options (Envolve) Dental Program. Members may continue to see their same dental provider if that provider is also contracted through Envolve Dental’s network. If their current dental provider is not contracted with Envolve, the member may select any in-network dental provider for covered services.
- The Pharmacy Network is very similar so most members will continue to get prescriptions filled at their current retail pharmacy. Members utilizing specialty pharmacy medications will be notified in advance if their pharmacy is no longer in the network.
- Non-emergent transportation services. Care1st currently partners with MTBA and AzCH-Complete Care Plan partners with Veyo. However, effective October 1, AzCH-Complete Care Plan will also partner with MTBA and will no longer work with Veyo. Therefore, Care1st members transitioning to AzCH-Complete Care Plan 10/1/21 will have no change in their non-emergent transportation provider.
- Routine vision services will transition to Envolve Benefit Options (Envolve) Vision Program. Members will continue to see their same vision provider if that provider is contracted with Envolve Vision’s network. If their current vision provider is not contracted with Envolve, they may select any in-network vision provider for covered services.
- Answer: Care1st and AzCH-Complete Care Plan have been working to minimize any impact to Care1st members. Most Care1st members will have access to their same providers. However, some members may need to be assigned to a different PCP or end up transitioning to a different specialist provider. If a member is assigned to a different PCP or Dental Home, they will be notified in writing in October. Some differences between the Care1st and AzCH-Complete Care Plan networks include:
- Question: Will all Care1st members automatically move to AzCH-Complete Care Plan?
- Answer: This is seamless for members. Members did not have to do anything to effectuate this change. All impacted members had the opportunity to choose a different AHCCCS plan during a special choice period in July. Care1st members that did not choose another plan during the special choice period will automatically become AzCH-Complete Care Plan members effective 10/1/21. Approximately 105,000 Care1st members will become AzCH-Complete Care Plan members.
- Question: Will Care1st members’ health plan benefits change due to the transfer?
- Answer: No. All AHCCCS health plans provide the same covered services to its members as required by law and contract.
- Question: Will Care1st members receive new Member ID cards?
- Answer: Yes, Care1st members will receive an ID card from their new plan within 12 business days of October 1st. An example of the AzCH-Complete Care Plan ID card is below.
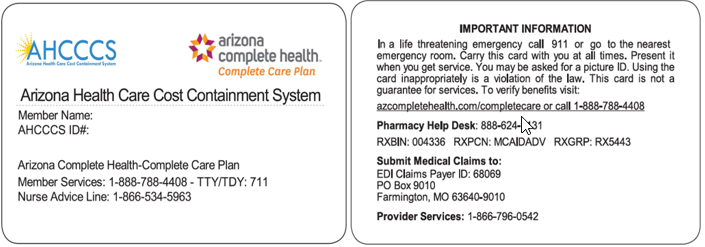
- Answer: Yes, Care1st members will receive an ID card from their new plan within 12 business days of October 1st. An example of the AzCH-Complete Care Plan ID card is below.
- Question: Where do I submit claims for members?
- Answer: You should submit claims for services rendered prior to 10/1/21 to Care1st. Claims for services rendered on or after 10/1/21 for AzCH-Complete Care Plan members should be submitted to AzCH-Complete Care Plan. AzCH-Complete Care Plan encourages you to submit claims electronically through Availity. Our payer ID is 68069.
- Paper Claims may be mailed to:
Arizona Complete Health-Complete Care Plan
PO Box 9010
Farmington, MO 63640
Additional details on claims submission included in our separate Billing Communication (1st distribution date = end of August)
- Paper Claims may be mailed to:
- Answer: You should submit claims for services rendered prior to 10/1/21 to Care1st. Claims for services rendered on or after 10/1/21 for AzCH-Complete Care Plan members should be submitted to AzCH-Complete Care Plan. AzCH-Complete Care Plan encourages you to submit claims electronically through Availity. Our payer ID is 68069.
- Question: What services require prior authorization (PA)?
- Answer: The AzCH-Complete Care Plan Pre-Auth Check tool is available at on our website: www.azcompletehealth.com > For Providers > Pre-Auth Check. Please use this tool to determine if PA is required. You can submit PA requests online via our secure Provider Portal or by fax.
- Question: If I obtained a PA from Care1st for a medical or behavioral health service prior to the transition, must I request a new prior authorization from AzCH-Complete Care Plan?
- Answer: No. Care1st will share all open (unused) PAs with AzCH-Complete Care Plan. AzCH-Complete Care Plan will honor these PAs through the expiration date or 11/30/21, whichever comes first.
Although the AzCH-Complete Care Plan PA Team is responsible for the majority of PAs, AzCH-Complete Care Plan works with outside partners for review of PA for certain services. Those partners, listed below, will also honor the open Care1st PAs.- Chiropractic Services: ASH. ASH will honor open PAs through the expiration date or 11/30/21, whichever comes first https://ashlink.com (800) 972-4226.
- Complex imaging, MRA, MRI, PET, and CT: NIA. NIA will honor open PAs through the expiration date or 11/30/21, whichever comes first. https://www1.radmd.com/radmd-home.aspx (800) 327-0641.
- Dental Services: Envolve Dental. Envolve Dental will honor open PAs through the expiration date or 11/30/21, whichever comes first. https://dental.envolvehealth.com/ (844) 876-2028.
- Orthopedic Procedures: Turning Point. Although Turning Point reviews requests, the PAs are then entered into the AzCH-Complete Care Plan system for claims payment. Open Care1st PAs for these service will be honored through the expiration date or 11/30/21, whichever comes first http://www.tpshealth.com/ (480) 865-2486.
- Oncology/Supportive Drugs: New Century. New Century will honor open PAs through the expiration date or 11/30/21, whichever comes first. https://my.newcenturyhealth.com (877) 624-8601.
- Vision Services: Envolve Vision. Care1st does not require PA for vision service. Envolve Vision is responsible for preventive services screenings and hardware. No PA is required for par providers https://visionbenefits.envolvehealth.com/ (844) 610-0177.
- Answer: No. Care1st will share all open (unused) PAs with AzCH-Complete Care Plan. AzCH-Complete Care Plan will honor these PAs through the expiration date or 11/30/21, whichever comes first.
- Question: What if I don’t have an existing open PA and am providing a service 10/1/21 and after to a former Care1st member, now AzCH-Complete Care Plan member?
- Answer: If you are not a participating (non-par) provider with AzCH-Complete Care Plan, like all non-par providers, a PA is required for all services. You may submit a PA request via fax or register for our secure portal and submit the request electronically through the portal.
- Answer: If you are a participating (par) provider with AzCH-Complete Care Plan, you should determine if a PA is needed before providing the service by using our PA Look Up Tool on our web site: https://www.azcompletehealth.com/. If a PA is needed, you may submit a request via the secure web portal or fax.
- Question: If a pharmacy PA was obtained for medication from the Care1st Pharmacy team prior to the transition, must I request a new pharmacy PA from the AzCH-Complete Care Plan Pharmacy team?
- Answer: No. Care1st will share open pharmacy PAs with AzCH-Complete Care Plan. AzCH-Complete Care Plan will honor the open pharmacy prior authorizations through the expiration day or 9/30/2022, whichever comes first.
- Question: If I’m not in the AzCH-Complete Care Plan network, may I request a PA to see a former Care1st, now AzCH-Complete Care Plan, member?
- Answer: If you are not in the AzCH-Complete Care Plan network, you may request a PA for continuity of care. Your request will follow the out of network review process and you will be notified if the service request is approved or denied. Please use the Medicaid AzCH-Complete Care Plan PA Form. You may also contact the Provider Call Center for a hard copy of these documents. Please provide all pertinent clinical information including current treatment plan with your request.
- Question: What products does AzCH-Complete Care Plan offer?
- Answer: AzCH-Complete Care Plan serves traditional Medicaid, CHIP members and Medicare Dual SNP members in Maricopa, Pinal, Gila, Cochise, Graham, Greenlee, La Paz, Pima, Santa Cruz, and Yuma counties. Care1st members transitioning to AzCH-Complete Care Plan who also have Medicare coverage have the option of enrolling in Wellcare by Allwell, Arizona Complete Health’s Medicare offering, to be in an aligned plan. Members who want to enroll in Wellcare by Allwell may contact the Medicare Sales Center at (866) 850-7255.

For additional updates regarding the Care1st member migration to Arizona Complete Health-Complete Care Plan, please visit the new Member Transition webpage where you can ask questions or provide feedback!

