C3 Action Event Primer
Setting the Stage for the Community Consensus Collaborative (C3) Action Event
Laying the Foundation – C3 Lead-Up Events
Arizona Complete Health-Complete Care Plan held C3 Lead-Up events to gather ideas from the community – with input from 365 people. C3 Lead-Up events were:
- C3 Civic Leadership Development training for peers and family members, hosted by the Arizona Peer & Family Coalition (39 participants)
- C3 Stigma Roundtable with Adult System of Care Providers (30 participants)
- C3 Arizona Dialogue on Stigma in the Workplace with Peer Support Specialists, Family Support Providers, Peer/Family-Run Organization leaders, and Health Home clinical leaders (32 participants)
- C3 Community Roundtable on Value & Outcomes with peers and family members (4 participants)
- C3 Peer/Family Provider Roundtable on Value & Outcomes with the Peer & Family Support TA Collaboration (10 participants)
- Arizona Complete Health-Complete Care Plan Medicaid Plan President spoke at the Arizona Peer & Family Coalition’s Mental Health Monday – SUCCESS: Defined and Discussed (5 panel members and 15 participants)
- C3 Community Survey sent to members, families, providers, and partners (229 participants)
The C3 Action Event takes the feedback and ideas gathered through Lead-Up events and turns it into a plan of action. The thoughts shared through Lead-Up Events helped shape the C3 Action Event.
The following is a summary of each lead-up event.
With the Arizona Peer & Family Coalition and Hope, Inc., Arizona Complete Health-Complete Care Plan offered a C3 Civic Leadership Development class for 39 peers and family members. The class helps peers and family members learn to share their voices. The C3 Civic Leadership Development class covers:
- Mental health and the recovery movement
- Systems and structures
- Sharing your story
- Ways to fight for mental health rights
Attendee comments:
- I feel really rejuvenated by the work I have done and hope I can help others.
- We appreciated having our stories and voices heard.
- Very helpful presentation. Thank you.
- I hope you will allow me to continue to be part of the group.
- The actual exercise of writing our story was key.
C3 Civic Leadership Training Evaluation Results:
- 100% of attendees said they will advocate for themselves or a loved one.
- 85% will speak with a policy maker.
- 100% will share their story.
- 85% will join a committee.
C3 Civic Leadership Training Evaluation Results:
- 100% of attendees said they will advocate for themselves or a loved one.
- 85% will speak with a policy maker.
- % will share their tory.
LeC3adership Training Evaluation Results:
- 100% of attendees said they will advocate for themselves or a loved one.
- 85% will speak with a policy maker.
- 100% will share their story.
- 85% will
The Arizona Complete Health-Complete Care Plan Adult System of Care providers discussed how stigma can lead to people not getting the care they need. Provider leaders said stigma deeply affects starting treatment. Specialists may not accept referrals due to stigma. Attendees also talked about the stigma of medication assisted treatment (MAT). There is a wrong belief that “it is just replacing one drug with another and/or trading one addiction for another”.
Attendees shared thoughts on what is working to help reduce stigma and what else can be done:
- More health education programs for people with mental illness and families.
- Help family members become an active part of treatment.
- More focus on building trust with the family.
- Make mental health a normal part of dialog.
- Address limits around talking about substance use in schools. More prevention education in schools. Prevention education should begin at 11-12 years old.
- A Medical Director that provides monthly training on MAT has lowered stigma for one health home.
- Keep strong relationships with first responders.
- Being a Narcan supply site gives providers the chance to talk to people when they come in to pick up Narcan. This creates more chances to connect and get people into treatment.
The AZ Dialogue focused on stigma in the workforce. Attendees included Behavioral Health Home Clinicians, staff in leadership roles, Peer/Family Run Organization CEOs and Peer & Family Support staff at Behavioral Health Homes and Peer/Family Run Organizations. The group discussed ways to fight stigma and the value of self-disclosure. Peer support specialists shared their experience with stigma in their personal lives as well as from co-workers and supervisors at work. People in roles that ask for self-disclosure still experience stigma within their jobs. The group shared personal views, listened to one another’s experiences, and created space for ideas. Below are items discussed during the C3 AZ Dialogue:
Strategies for Removing Stigma at Work
- Peer Support training should focus on the soft skills of working in an office.
- Create a standard certification test for peer support specialists. This may increase respect for the role.
- Person-centered speech matters!
- Require health plans and providers to hire peer support specialists. Note the importance of people with lived experience in all roles.
- Share peer success stories. People can find hope from stories of success. Professionals in healthcare can overcome bias by hearing more success stories.
- Teach HR departments about the role of peer and family support. Remove policy barriers related to self-disclosure. Promote the use of self-disclosure as a tool for building rapport.
- Value starts with higher pay. Review pay scales for peer and family support professionals. Compare it to other helping professionals and healthcare workers. Make the range of pay fair. Create career ladders for peer and family support professionals.
- Educate healthcare professionals about the recovery model early in their career. Include peers and family members as presenters in college courses.
- Peer support specialists should be assigned at every entry point in the mental health system. Peer support is a great tool for removing stigma. When people who are struggling to ask for help meet someone in recovery, it gives hope and lessens stigma.
This event included four Arizona Complete Health-Complete Care Plan members and family members. The topics discussed were Value-Based Purchasing, member engagement, provider burn-out, and how to measure success. Group members did not have any experience with Value Based Purchasing. They suggested that peers and family members should be involved in these conversations and help define success. They also suggested that peers and family members be given more information and data about their own health and how to improve it.
The following are a few highlights from the roundtable:
- There are many ways to measure if a person is getting healthier. These include increased well care, more use of peer support, changes in physical activity, volunteering, community involvement, and the ability to show gratitude.
- Tests/lab work should be explained to members so they know what doctors are looking for. This can help them understand how mental and emotional state affects physical health. Members should have access to test results/lab work to track progress.
- Data that could help people stay healthy if it were shared includes:
- Info on why certain services are important and suggested.
- Access to lab work to see and track improvements in health. This includes paper and electronic copies.
- To help people start and stay in services, providers should follow-up, refer to in-network providers, and provide a restful setting.
- Offer an accountability partner that meets with members once a week.
- Members need help knowing what questions to ask.
This meeting is held by the Arizona Complete Health Office of Individual and Family Affairs (OIFA) team for all Family Support Providers and Peer Support Specialists in the Arizona Complete Health network. This is a meeting for problem solving and supporting one another. The C3 Action team joined the March meeting to discuss stigma. Below are thoughts shared in the meeting.
Ways stigma shows and acts as a hurdle to getting services:
- Cultural views are not respected. Example: An American Indian member was not able to bring his medicine bag with him to a treatment facility.
- Communication styles should be flexible. Example: An older family member was treated differently when she asked for a phone call rather than an email.
- Choices of members in transition (from their assigned birth gender) are not being respected. Providers are refusing to call them by their chosen name.
What is working?
- Family Support Providers help remove stigma by sharing stories. It helps when we can meet the person where they are.
- Having another person in the room as an advocate helps you to not feel stigma and not feel ignored.
- Diversity Equity and Inclusion Committee – be willing to have “Courageous Conversations” and discuss ways to improve.
- OIFA teams – everyone comes from lived experience. OIFA attendance on every committee and department throughout an organization has been helpful. Having the true member experience in all lines of business helps to remove stigma.
Other Ideas:
- Ensure there is a peer/family support face upon intake.
- Be welcoming. Offer people water/comfort as soon as they get in the door.
- Get out in the community to educate and connect people with care and support.
- Get more youth peer support certified. Provide youth with chances to share their stories.
- One youth said his greatest chance was being able to go and share his story at a conference. This opened a whole new world for him. He got to travel to a new state to speak at the conference.
James Stover, Medicaid Plan President at Arizona Complete Health-Complete Care Plan spoke at the Arizona Peer & Family Coalition’s Mental Health Monday. The panel was a mix of providers, peers and family members. They discussed what success means for a member versus what it means for a provider or a health plan. This event was held by the Arizona Peer & Family Coalition and NAMI Yavapai County. There were many answers to the question of what success looks like. Key points that the group agreed on included: people meeting/keeping recovery goals, people being respected, feeling safe, and meeting goals and financial plans. Below are some thoughts shared:
What does success look like?
- “Success looks like psychological safety in our communities. Until it is safe to have a mental illness, be a justice involved person, we are not going to have a safe recovery.”
- “Community members get permissions from the government to stigmatize and discriminate: if the gov discriminates against you, then the community has the right to discriminate. We are socially conditioned to discriminate Legitimizing dehumanizing people.”
- “Success is reducing the stigma. Don’t treat people like they are terrible humans if they have a drug problem.”
- “The more people aware of the services the more people can get help.”
- “Providers have employees with a criminal justice background. They started at the bottom, and they now hold management positions running statewide programs. That is success.”
- “Financial sustainability is ensuring people get the right levels of care.”
- “Success is meeting people where they are, which has to do with engagement, and no other places are better at engagement than those at Peer/Family Run Organizations (PFROs).”
- “Advocate: making sure peer & family members are at the table.”
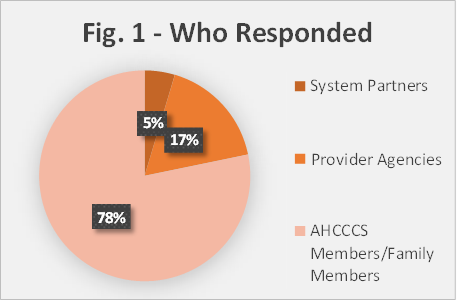
The Community Survey link was shared with members, families, providers, and community partners. The survey contained three main parts: value-based purchasing, data, and stigma. We received 229 responses. Below is a summary of the results:
- Over 50% of people surveyed agree or strongly agree with the following: The health care system does a good job outreaching and getting individuals to come in for preventive screening appointments.
- Social determinants of health (SDOH) that most affect the health of members were reported as: safe housing and neighborhoods, education, job opportunities, and income.
- Over 50% of participants agree or strongly agree that the health care system does a good job getting people to come in for preventive screenings.
- Over 50% of providers and 100% of system partners agreed that Value Based Purchasing is important.
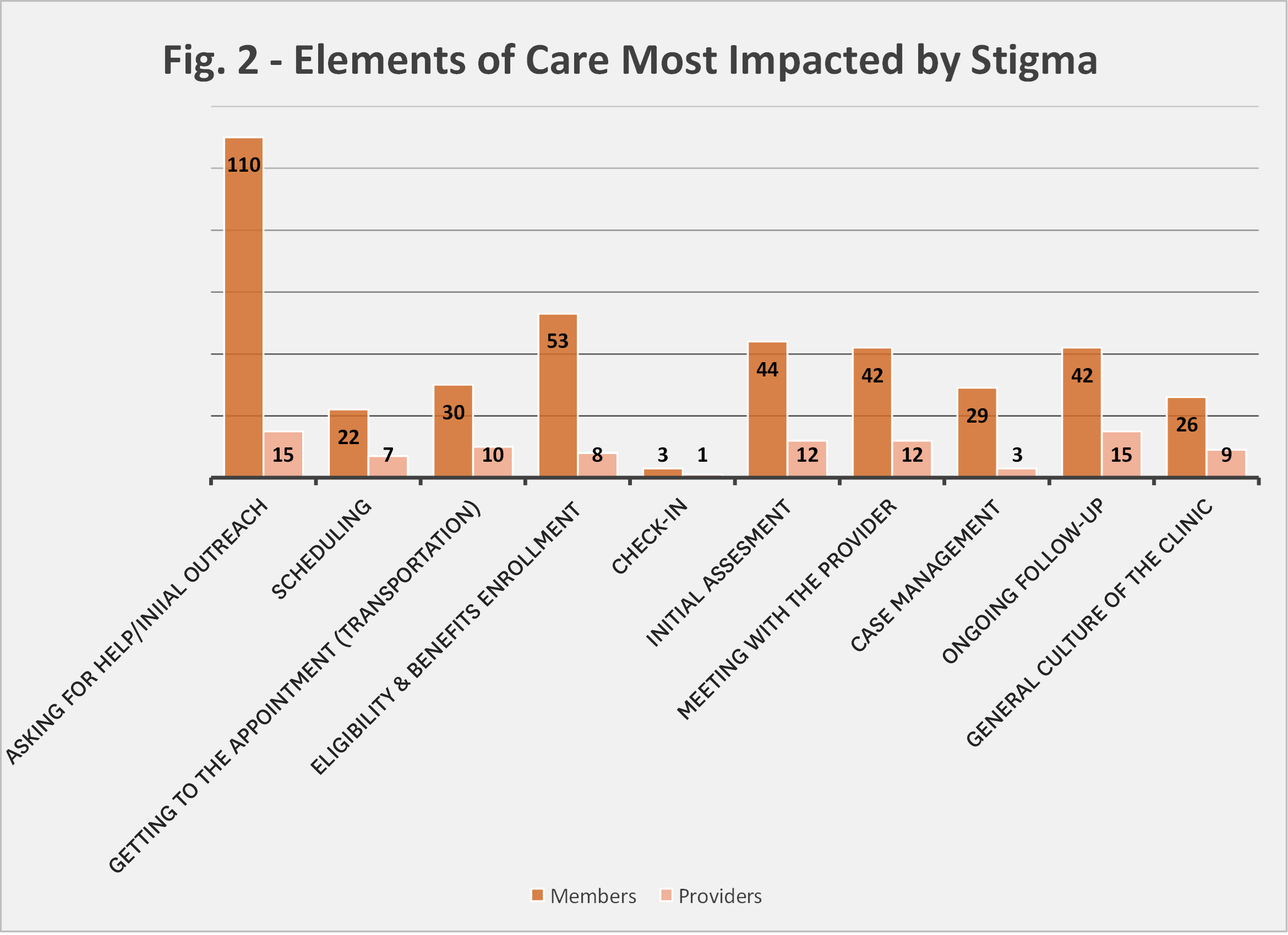
- Providers shared that the top areas affected by stigma are deciding to ask for help and ongoing follow-up for treatment. Members agree, stating that stigma is an issue when deciding to ask for help/look for treatment. See the full comparison between responses in Figure 2.
What Survey Participants are Saying:
- “Increase education around mental illness for school-aged youth to stop stigma while young. Making people understand SMI determinations doesn’t mean dangerous or scary, just extra care; just as with diabetes.”
- “Get members more involved with their care, ask them for input.”
- “We need to see less about the people that are engaging in criminal activity's mental health. We need to stop
- making it seem as only those (or all of those) with mental health issues are engaging in crimes.”
- “Talk openly about mental health, educate our staff, share experiences, and be conscious of how we talk to
- individuals-not making individuals feel like they are non-humans.”
- “We need initiatives to change the way the community talks about people with SUD-- moving away from
- terminology like junkie to helping people understand the efficacy of MAT and having more empathy.”
- “Educating the public regarding behavioral health diagnosis, emphasizing that a BH diagnosis is the same as other medical diagnoses, such as heart disease or diabetes and should be treated as such. Encourage people to ask questions.”

